| Essential topics/experience:
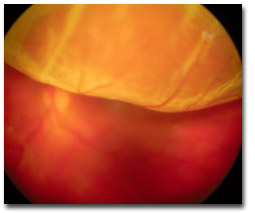
To have become familiar with the following: i. Flashes and floaters: complications
of posterior vitreous detachment and recognition of
ii. Vitreous haemorrhage: from retinal tears or neovascularisation; initial management. iii. Retinal detachment: classification, predisposition, recognition and urgency of treatment; recognition of proliferative vitreoretinopathy. iv. Senile/acquired retinoschisis: recognition. v. Liaison: with low vision services. Practical skills:
i. Scleral indentation with indirect ophthalmoscopy. ii. Retinal drawing. iii. Cryopexy and laser (via slit-lamp and indirect ophthalmoscope delivery systems) for retinal tear. Background theory/principles:
i. B-Scan ultrasound for opaque media. ii. Vitreoretinal surgery: including closed intraocular microsurgery, scleral buckling and internal tamponade. iii. Intraocular foreign body: complications and management. iv. Other vasoproliferative vitreoretinopathies including sickle cell retinopathy, retinopathy of prematurity, Eales’ disease. v. Genetic vitreoretinal disease: Stickler syndrome. X-linked retinoschisis. vi. Asteroid hyalosis. vii. Choroido-retinal coloboma. |
|||
|